Heart attacks continue to be dangerous for years.
What they tell you when you leave the hospital:
You’ll be OK if you take these medications and make these lifestyle changes.
what they don't tell you:
Your prognosis. Watch this video: What to do after a heart attack.
you survived a heart attack.
what are the most important questions you should be asking?
In this video we expose the two different meanings of the term “blockage” and how to know which type of blockage someone is talking about.
Then we explore one of the most important questions any heart attack survivor can ask: “What causes heart attacks?”
Because this idea is so foundational, so central to an effective prevention program, it’s a long video (7 minutes).
Let us know if you think it’s helpful. We’d love to get your feedback with your comments or by sharing your thoughts with us by clicking on the contact us button below.
Below we’ll raise more questions that every heart attack survivor should be asking. (Scroll down below the EKG.)
What risks do you face after a heart attack?
Quite often heart attack survivors are not told about the risks they face. (1,2)
Some of the stats are listed below. But this is just a brief summary. The video above (WHAT TO DO AFTER A HEART ATTACK) has more details about different types of heart attacks and how they make a difference in gender-specific outlook or prognosis, especially in the first 30 days.
1-year mortality rate (45 and older):
1 of 4 women (23%) and 1 of 5 men (18%) will die within 1 year after a heart attack (see reference 3 below, ePage 493).
5-year mortality rate (45 and older):
1 of 3 men (36%) and 1 of 2 women (47%) will die within 5 years after a heart attack. (ref 3, e493).
8-year mortality rate:
1 of 2 men and about 65% of women die within 8 years of a heart attack. (3)
“ We have a 100% survival rate after a heart attack.
”
What makes us different?
After learning their prognosis and what causes heart attacks, most heart attack survivors ask “How can I reverse my artery disease?”
The first step is to find out the answer to this question: “What caused my heart attack?”
Once we know what caused it, we’ll know exactly what to do to fix it.
Cholesterol is one risk factor. Blood pressure is another. So if you’ve had a heart attack and your doctor started a statin, a blood pressure pill and a blood thinner, take them.
There are over 20 modify-able risk factors.
What else hasn’t been tested for?
You’ll never know what caused your heart attack until you’ve tested for all modify-able risk factors and you’ve identified every single one causing the inflammation in your arteries. Click here to see our page on risk factors.
Is COVID a risk factor for heart disease?
COVID causes inflammation in the heart muscle, and also in the lining of the artery wall. That lining (called “endothelial cells”) can be affected by COVID long after the COVID is gone. (5, 6)
One study compared 153,000 COVID survivors to two large matched control groups without COVID. Within a year after a COVID infection, the risk of cardiac arrest was multiplied almost 2.5-fold. Heart attack risk was increased by 63%. The risk of myocarditis (inflammation of the heart muscle) was increased 5-fold. Risk was increased for all CV diseases/events studied. Risk was highest for those admitted to a hospital or treated in an ICU. (7)
When should testing begin?
We believe a thorough process of testing should begin immediately after the heart attack.
We’ll help you ask the right questions. And find real answers. Until you know what caused it, you’ll never know what to do about it.
OUR PROCESS WORKS:
Because we identify every risk factor needing attention.
Some doctors tell their patients “You can’t reverse artery disease.”
You cannot reverse it until you identify and treat every factor that caused it.
We help people reverse their artery disease every day.
Artery disease can be reversed!
Here are a couple of examples:
Having had 3 heart attacks and 6 stents in 5 years, this patient was on statins, blood pressure meds and blood thinners.
Then he had the “big one”
The most severe and dangerous heart attack of all, a STEMI (ST elevation MI). Cardiologists didn’t know what else could be done.
He contacted us. This ultrasound was done 6 weeks after the STEMI, before starting our program:
You can see the soft dangerous type of plaque that is vulnerable to rupture.
after testing for all modify-able risk factors, what did we do?
We changed his treatment plan. What did he do? He made the lifestyle changes we recommended and signed up for our management program.
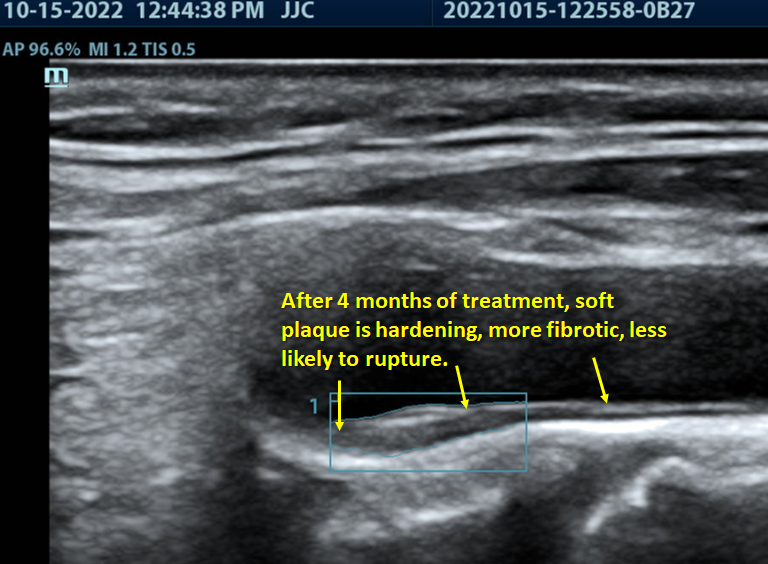
AFter 4 months of treatment at cardiosounD:
Here is the same arterial plaque 4 months later, now starting to harden like scar tissue.
Arteries have improved. Plaque is not as thick.
In 5 arteries tested, he’s had plaque regression (shrinking) by 11%.
As arteries improve, risk improves.
This patient is feeling great!
He did everything right
Before this patient had a heart attack, he did everything he was told to do to prevent heart problems. His first heart attack was a “Widowmaker” and he got a stent.
He asked what could be done to reverse this process. His cardiologist answered “You cannot reverse artery disease.”
He contacted us. This arterial ultrasound was taken one month after the heart attack.
Calcified plaque is easy to see. The soft dangerous (“vulnerable”) plaque is very faint, not easy to see in this picture.
after extensive testing for modify-able risk factors
We discovered problems he never knew about. We showed him what could be done with a new treatment plan to alter the course of his life. He made significant lifestyle changes.
After almost 4 months, his plaque thickness in 5 arteries has improved by 7%. Due to fibrosis and scaring, his soft plaque is now easier to see. Calcified plaque is more heavily calcified. Event risk is reduced.
“What can I do right now to make sure I never have another heart attack?”
start the testing process asap. Our process is simple: 3 easy steps.
STEP 1: Set up a FULL EVALUATION to determine every single factor that caused your heart attack. It’s not just about cholesterol.
STEP 2: Initiate blood biomarker and genetic testing right where you are. We can draw blood anywhere in the U.S.
STEP 3: Come to Atlanta for your baseline ultrasound study and consultation to review your test results with Dr. Hight. You’ll understand every factor that caused your heart attack. And once you know what caused it, you’ll know what to do about it.
When you address every risk factor, and then see your arteries getting better, you’ll be glad you came!
you’ll know you can live without fear.
reFERENCEs
Dracup K, et al. Acute coronary syndrome: what do patients know? Arch Intern Med. 2008; 168: 1049-1054.
Leifheit-Limson EC, et al. Sex differences in cardiac risk factors, perceived risk, and health care provider discussion of risk and risk modification among young patients with acute myocardial infarction: the VIRGO study. J Am Coll Cardiol. 2015;66:1949-1957
Virani, et al, Heart disease and stroke statistics- 2020 update: a report from the American Heart Association. Circulation. Mar 3, 2020. 141;9
Hight, T, unpublished data: Compared to population data (ref 3), Dr. Hight’s MI survivors have a 100% survival rate at 1 year, 5 years, and at 8 years, statistically significant (p < 0.05) for both genders at 1 year, and for males at 5 and 8 years.
Bernard, I, et al. Endothelium infection and dysregularion by SARS-CoV-2: Evidence and caveats in COVID-19. Viruses 2021, 13,29
Vosko, I.; Zirlik, A.; Bugger, H. Impact of COVID-19 on Cardiovascular Disease. Viruses 2023, 15, 508. https://doi.org/10.3390/v15020508
Xie, Y., et al. Long-term cardiovascular outcomes of COVID-19. Nat. Med. 2022, 28, 583–590